Mouth ulcers are common, but not all “mouth sores” mean the same thing. A canker sore inside the cheek is usually harmless and not contagious, while a cold sore on the lip border can spread through close contact, and infections can signal something that needs treatment. The tricky part is that many different problems look similar in the mirror, so knowing a few simple clues can help you decide what’s normal and what needs a dental visit.
This guide helps you tell the difference between canker sores, cold sores, infection-related ulcers, and explains the red flags that mean you shouldn’t wait. You’ll learn quick identification tips based on location, appearance, and healing time, plus what you can do at home for relief. If you’re in Kathmandu, we’ll also cover when to see a dentist and what to expect during an exam.
Mouth Ulcers Basics: What They Are and How to Quickly Identify the Type
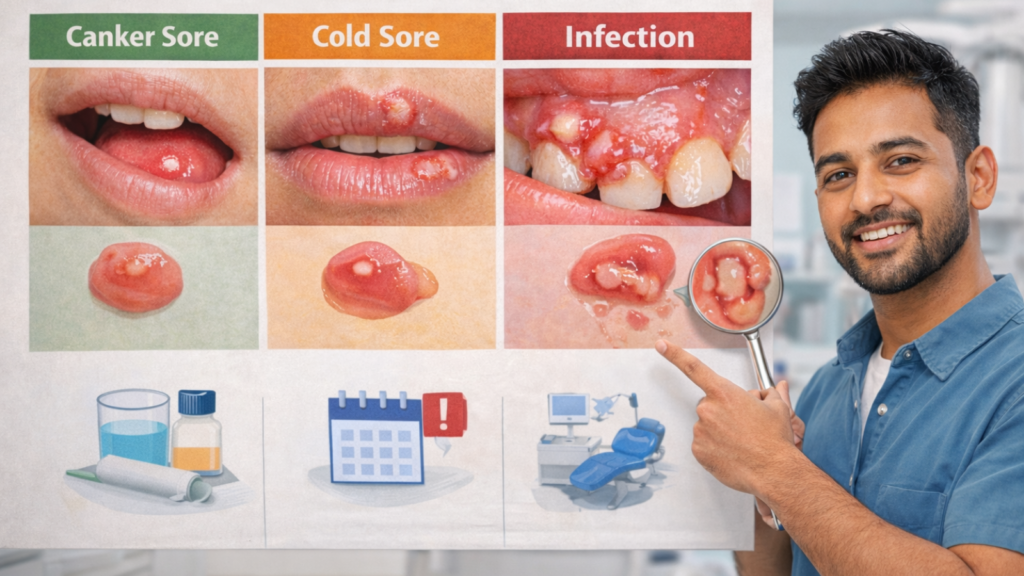
Most mouth ulcers are small breaks in the lining of the mouth caused by irritation, inflammation, or viral triggers. Location and appearance give the fastest clues, ulcers inside the mouth are often canker sores, while blisters and crusting on the lip border are more typical of cold sores. The timeline matters too: many heal in 7–14 days, but any sore lasting more than 3 weeks needs an exam.
Ulcer vs Blister vs “Sore”: Simple Definitions (and Why People Confuse Them)
An ulcer is an open wound in the mouth lining, while a blister is a fluid-filled bump, and “sore” is a general term for any painful spot. People confuse these terms because blisters often break and become ulcers within hours. A cold sore starts as a blister on your lip border, then ruptures into an ulcer. A canker sore appears directly as an ulcer inside your cheek. The distinction matters because blisters (especially cold sores) spread through contact, while most ulcers do not.
The confusion happens for 3 reasons: firstly, both cause pain; secondly, blisters quickly ulcerate and look identical to other ulcers; thirdly, people use “sore” interchangeably for any mouth pain. Knowing the starting form (blister vs direct ulcer) helps identify the cause.
Location and Appearance Clues: Inside Cheeks/Lips, Gums, Tongue, Lip Border (With Examples)

Location reveals the ulcer type faster than any other clue. Canker sores appear inside the mouth (inner cheeks, inner lips, tongue edges, soft palate, gums) where skin does not touch outside air. Cold sores cluster on the lip border (vermillion border), the outer edge of lips, or just outside the mouth where lip skin meets facial skin. Infections and trauma-related ulcers can occur anywhere, but bacterial abscesses concentrate near teeth, and fungal infections (thrush) favor the tongue and inner cheeks.
Appearance differences:
- Canker sores: round or oval, white or yellowish center, red halo, clean edges, 2 to 8 millimeters (mm) diameter
- Cold sores: grouped tiny blisters that merge, weep clear fluid, then crust over; occur on lip edge or just outside
- Infections: irregular shape, white patches (fungal), pus drainage (bacterial), or painful red swelling near a tooth
Trauma ulcers from sharp teeth or braces match the shape of the irritant (linear scrape from a sharp edge, round from a poking wire). You notice these occur at the exact contact point with the tooth or appliance.
Canker vs Cold Sore vs Infection: Quick Comparison Table (Contagious, Look, Cause, Timeline)
| Feature | Canker Sore | Cold Sore | Infection (Bacterial/Fungal) |
| Contagious | No | Yes (highly) | Sometimes (depends on cause) |
| Location | Inside mouth only | Lip border, outside mouth | Anywhere (gums, tongue, throat) |
| Appearance | Round ulcer, white center, red ring | Blisters→crust, clusters | White patches (fungal) or pus/swelling (bacterial) |
| Cause | Stress, trauma, diet, deficiency | Herpes simplex virus (HSV-1) | Bacteria, yeast (Candida), other viruses |
| Pain level | Moderate to severe | Moderate, burning sensation | Varies (burning, throbbing) |
| Timeline | 7 to 14 days | 7 to 10 days (blister to heal) | Depends on treatment; thrush needs antifungals |
This table gives you a first-pass diagnosis, but overlaps exist. A cold sore can spread to inside the mouth (rare), and herpetiform canker sores mimic cold sore clusters but stay inside the mouth and are not contagious.
Normal Healing Timeline: 7 to 14 Days vs the “3-Week Rule” (When Persistence Becomes a Concern)
Most benign mouth ulcers heal within 7 to 14 days without treatment. Canker sores peak in pain around day 3 to 4, then gradually shrink. Cold sores scab by day 5 to 7 and fully heal by day 10. Trauma ulcers from accidental bites resolve in 5 to 7 days once the irritation stops.
The “3-week rule” is a critical safety marker: any ulcer lasting longer than 3 weeks requires professional examination. Persistence beyond 21 days suggests deeper causes (immune dysfunction, chronic irritation, nutritional deficiency, or pre-cancerous change). Dentists and doctors in Kathmandu use this threshold to decide when to biopsy. You should mark the ulcer’s start date and book an appointment if it remains unchanged or enlarges past 3 weeks.
Canker Sores (Aphthous Ulcers): The Most Common Non-Contagious Mouth Ulcer

Canker sores are painful, round or oval ulcers that usually appear inside the cheeks, lips, or under the tongue and are not contagious. They often flare with stress, minor trauma (biting), spicy/acidic foods, or certain toothpastes, and they typically heal on their own. If you get them frequently or they’re large and slow to heal, it’s worth checking for nutrient deficiencies and underlying conditions.
Classic Canker Sore Pattern and Top Triggers (Stress, Trauma, Spicy/Acidic, Sodium Lauryl Sulfate Toothpaste)
Canker sores are recurrent, non-contagious ulcers that form inside the mouth due to immune-mediated inflammation, not infection. You wake up with a tender spot that becomes a round, painful ulcer within 24 hours. The exact cause remains unclear, but the condition runs in families and flares with specific triggers.
Top 5 triggers we see in Kathmandu patients:
- Stress and fatigue: exam periods, work deadlines, family events
- Mouth trauma: accidental cheek bites, aggressive brushing, sharp tooth edges
- Spicy and acidic foods: excessive chili (khursani), tomato-heavy curries, citrus fruits
- Sodium Lauryl Sulfate (SLS) in toothpaste: foaming agent that irritates mucosa in sensitive people
- Hormonal shifts: menstrual cycle changes in women
Switching to SLS-free toothpaste reduces recurrence by 30 to 50 percent in people with frequent canker sores. Keeping a trigger diary (food, stress level, ulcer appearance) reveals personal patterns most patients overlook.
Types That Matter: Minor vs Major vs Herpetiform (Size, Pain, Healing Time)
Three types exist, based on size and severity:
- Minor aphthous ulcers (80 percent of cases): 2 to 8 mm diameter, shallow, heal in 7 to 10 days without scarring; most people get 1 to 3 ulcers per flare
- Major aphthous ulcers (10 to 15 percent): >10 mm diameter, deep, extremely painful, take 2 to 6 weeks to heal and may scar; often occur on soft palate or throat area where swallowing becomes difficult
- Herpetiform aphthous ulcers (5 percent): clusters of 10 to 100 tiny ulcers (1 to 2 mm each), mimic herpes but are not viral or contagious; heal in 7 to 14 days
Major ulcers warrant a dental visit because pain interferes with nutrition, and prolonged healing raises infection risk. Herpetiform ulcers cause diffuse mouth pain and are often misdiagnosed as cold sores, but the inside-mouth-only location and non-contagious nature confirm the difference.
Recurrent Ulcers: Nutrient Deficiencies (B12/Iron/Folate), Gut Issues, Immune Causes, When to Test
Frequent canker sores (more than 4 to 6 episodes per year) signal underlying issues. Nutrient deficiencies are the most correctable cause: low vitamin B12, iron, or folate impairs mucosal repair, triggering ulcers. Vegetarians and people with poor absorption (celiac disease, inflammatory bowel disease) face higher risk.
When to request blood tests:
- Ulcers occur monthly or more often
- Family history of autoimmune disease (thyroid, lupus, Behçet’s disease)
- Associated symptoms: fatigue, pale skin, digestive issues, joint pain
A complete blood count (CBC), serum B12, ferritin, and folate panel costs NPR 2,000 to 3,500 in Kathmandu labs and identifies deficiencies in 20 to 40 percent of recurrent cases. Correcting deficiency with supplements (B12 injections, iron tablets) reduces ulcer frequency significantly within 2 to 3 months.
Immune-mediated conditions like Behçet’s disease cause severe, recurrent oral and genital ulcers plus eye inflammation. These cases need referral to a rheumatologist or internal medicine specialist for systemic treatment.
Cold Sores (Oral Herpes): Contagious Blisters That May Ulcerate

Cold sores usually start with tingling or burning, followed by clustered blisters that can break and crust, most often on the lip border. They are contagious, especially in the early blister/weeping stages, so avoiding kissing and sharing utensils helps prevent spread. Antiviral treatment works best when started early, ideally at the first tingling sensation.
The Early “Tingle” Phase and Stages: Blister → Weep → Crust → Heal (What’s Typical)
Cold sores result from herpes simplex virus type 1 (HSV-1) reactivation, a lifelong infection that stays dormant in nerve cells and flares during stress, fever, sun exposure, or immune suppression. The hallmark is the prodrome (early warning): you feel tingling, itching, or burning on the lip border 12 to 24 hours before blisters appear. This is the best treatment window.
Classic progression:
- Day 0 to 1 (prodrome): tingling, redness
- Day 1 to 2 (blister stage): small fluid-filled bumps cluster together
- Day 2 to 4 (weeping stage): blisters rupture, ooze clear fluid (highly contagious)
- Day 4 to 7 (crusting stage): yellow-brown scab forms, pain decreases
- Day 7 to 10 (healing): scab falls off, pink skin remains, fully healed by day 10 to 14
Starting antiviral medication (acyclovir, valacyclovir) during the prodrome or within 24 hours of blister appearance cuts healing time by 1 to 2 days and reduces viral shedding.
How Cold Sores Spread (and How to Prevent It): Kissing, Sharing Items, Touching Eyes
Cold sores are highly contagious from the blister stage until the scab completely falls off. HSV-1 spreads through direct contact with the sore or saliva. Common transmission routes in Kathmandu households include sharing water bottles, utensils, towels, or kissing children on the lips.
Critical prevention steps:
- Avoid kissing anyone (especially infants) when you have active blisters or crusts
- Do not share cups, straws, lipstick, or eating utensils
- Wash hands immediately after touching the sore or applying medicine
- Use disposable cotton swabs (not fingers) to apply topical creams
- Replace your toothbrush after the outbreak heals to avoid reinfection
Never touch your eyes after touching a cold sore. Transferring the virus to the eye causes herpes keratitis, a serious corneal infection that can damage vision. You reduce transmission risk by 80 percent simply by using hand hygiene and avoiding direct contact during active lesions.
Treatment That Works Best Early: Antivirals Timing, Pain Relief, and What to Avoid
Antiviral drugs (acyclovir 400 mg five times daily or valacyclovir 2 grams twice in one day) work best when started during the tingle phase or within 24 hours of blister appearance. Late treatment (after day 3) offers minimal benefit because the virus has already replicated. Kathmandu pharmacies stock generic acyclovir (NPR 15 to 25 per tablet); a 5-day course costs NPR 300 to 500.
Pain management and comfort:
- Over-the-counter pain relievers: paracetamol or ibuprofen
- Topical numbing gels: benzocaine or lignocaine gel (apply sparingly)
- Ice wrapped in cloth: reduces swelling and numbs pain (10 minutes per hour)
What to avoid:
- Popping blisters (increases infection risk and prolongs healing)
- Harsh alcohol-based mouthwashes on open sores (causes burning without benefit)
- Steroid creams without prescription (may worsen viral replication)
- Sun exposure without lip balm with SPF 30+ (UV triggers recurrence)
People with frequent outbreaks (more than 6 per year) benefit from suppressive antiviral therapy (daily low-dose valacyclovir), which reduces recurrence by 70 to 80 percent.
Infections and Other Look-Alikes People Call “Mouth Ulcers”
Some “ulcers” are actually infections like thrush (white patches and burning) or gum infections that can mimic sores and require targeted treatment. Viral illnesses such as hand-foot-mouth disease or shingles can cause multiple painful mouth lesions, often with fever or body symptoms. Persistent or unusual ulcers can also come from mechanical irritation (braces/sharp tooth), allergic reactions, medication-related sores, or immune conditions.
Thrush (Fungal): White Patches, Burning Tongue, Inhaler/Antibiotic Risks
Oral thrush is a yeast infection caused by Candida albicans overgrowth, appearing as white patches on the tongue, inner cheeks, or palate that wipe off to reveal red, raw tissue underneath. You experience burning or loss of taste more than sharp ulcer pain. Thrush differs from canker sores because the white coating is thick and removable (like cottage cheese), not a fixed white ulcer base.
High-risk groups in Kathmandu:
- Diabetics with poor blood sugar control
- Asthma patients using steroid inhalers without rinsing after use
- People on prolonged antibiotics (disrupts normal mouth bacteria)
- HIV/AIDS patients or those on chemotherapy
- Denture wearers with poor hygiene
Treatment requires antifungal medication (nystatin oral suspension or fluconazole tablets), not the usual ulcer gels. Steroid inhaler users prevent thrush by rinsing and spitting immediately after each puff, a step many skip because it seems unnecessary.
Bacterial Causes: Gum Infections, Abscess Drainage, and When Dental Treatment Is Needed
Bacterial infections create painful swelling, pus discharge, and sometimes ulcer-like openings near teeth. A dental abscess (pus collection from tooth infection) may drain through the gum, forming a pimple-like bump (gumboil) that bursts and looks like an ulcer. You also notice tooth pain, sensitivity to hot/cold, facial swelling, or fever.
Periodontal (gum) disease causes red, swollen gums that bleed and develop painful ulcerated areas between teeth. Severe cases produce a foul taste and loose teeth. Bacterial ulcers need dental treatment, antibiotics alone mask symptoms without fixing the infected tooth or gum pocket.
When to see a dentist immediately:
- Facial swelling or fever (risk of spreading infection)
- Severe, throbbing tooth pain with gum swelling
- Pus drainage or foul odor from a gum area
- Ulcer that appeared after dental work or near a filled/crowned tooth
At BrightSmile Dental Clinic in Putalisadak, we perform gentle drainage, root canal treatment, or gum cleaning as needed, often providing same-day relief for abscess pain. Ignoring dental infections leads to bone loss, tooth extraction, or systemic complications.
Viral Illnesses: Hand-Foot-Mouth, Shingles, Fever-Related Mouth Sores (Common Patterns)
Several viruses cause mouth ulcers as part of systemic illness. Hand-foot-mouth disease (HFMD), common in children under 5 years, produces multiple small ulcers on the tongue, inner cheeks, and throat, plus a rash on palms and soles. Fever and sore throat accompany the sores. HFMD is highly contagious but self-limiting (resolves in 7 to 10 days).
Shingles (herpes zoster) reactivation affecting the trigeminal nerve causes painful blisters on one side of the face, inside the mouth, or on the tongue, following nerve distribution. You notice severe, burning pain before blisters appear, and the one-sided pattern is diagnostic. Shingles requires urgent antiviral treatment (within 72 hours) to prevent nerve damage and postherpetic neuralgia.
Fever-related ulcers occur during high fever from flu, dengue, or typhoid. These are small, multiple, and heal once the fever resolves. They differ from recurrent canker sores by appearing only during systemic illness.
Other Causes: Sharp Tooth/Braces/Dentures, Burns, Allergies and Drug Reactions/Immune Blistering Conditions
- Trauma from sharp tooth edges, orthodontic brackets, or ill-fitting dentures creates linear or irregular ulcers at the contact point. The ulcer appears within hours of irritation and heals rapidly (3 to 5 days) once the sharp edge is smoothed or the appliance adjusted. Denture wearers develop chronic ulcers if the denture rocks or has rough spots; relining or remaking the denture solves the problem.
- Chemical or thermal burns from hot food (momos, tea), spicy chili paste, or accidentally biting into pani puri with excessive lemon cause immediate pain and white, sloughing tissue. The injured area ulcerates but heals in 5 to 7 days. Avoid the irritant during healing.
- Drug reactions to pain relievers (aspirin held against a tooth, causing chemical burn), antibiotics (sulfonamides), or chemotherapy agents produce diffuse, painful ulcers.
- Immune blistering conditions like pemphigus vulgaris cause large, fragile blisters that rupture into raw, widespread ulcers, often involving skin and eyes as well. These severe cases require specialist care (dermatologist or oral medicine).
When to Worry: Red Flags, Oral Cancer Concern, and What to Do in Kathmandu
You should book an exam if an ulcer lasts over 3 weeks, keeps returning in the same spot, grows larger, or feels unusually hard at the edges. Red flags include unexplained bleeding, numbness, a neck lump, difficulty swallowing, or weight loss. In Kathmandu, a dentist can check for trauma and infection and guide you if tests or specialist referral (ENT/oral medicine) is needed.
Warning Signs to Book an Exam: Ulcer >3 Weeks, Enlarging, Very Frequent, or Unusually Severe
Book a dental or medical exam if your mouth ulcer:
- Persists beyond 3 weeks despite home care
- Enlarges or changes appearance instead of healing
- Recurs more than 6 times per year without clear triggers
- Causes severe pain that prevents eating or sleeping
- Appears alongside other symptoms (weight loss, fatigue, night sweats, difficulty swallowing)
These patterns indicate the ulcer may not be a simple canker sore. Chronic non-healing ulcers raise concern for nutritional deficiency, immune disorder, chronic infection, or malignancy. Early evaluation prevents complications and identifies treatable causes.
Red Flags Checklist: Hard/Raised Edges, Unexplained Bleeding, Numbness, Neck Lump, Weight Loss
Seek immediate professional evaluation if you notice any of these red flags:
- Hard, raised, or rolled edges: benign ulcers have soft, flat margins; firm, raised edges suggest abnormal tissue growth
- Painless ulcer: most benign ulcers hurt; a painless, non-healing ulcer is suspicious for malignancy
- Spontaneous bleeding: ulcer bleeds without touching it or bleeds excessively when you brush nearby
- Numbness or tingling: loss of sensation around the ulcer or in the lip/tongue
- Neck lump: swollen lymph node that does not shrink within 2 weeks
- White or red patches nearby: leukoplakia (white) or erythroplakia (red) lesions adjacent to the ulcer
- Unintentional weight loss: losing weight without trying, alongside mouth sores
These signs do not confirm cancer but warrant urgent investigation. Oral cancer is curable when detected early (stage I survival >80 percent), but late-stage disease has poor outcomes. The most common risk factors in Nepal are tobacco use (smoking, chewing), heavy alcohol consumption, and betel quid (paan/gutkha) chewing.
Who to See in Kathmandu and What to Expect at the Visit (Dentist vs GP/ENT; Exam, Tests, Referral/Biopsy)
Start with a dentist for any oral ulcer concern. Dentists in Kathmandu are trained to diagnose oral lesions and perform biopsies. At BrightSmile Dental Clinic (Putalisadak), we examine the ulcer under good lighting, palpate surrounding tissue for hardness, check lymph nodes, and review your medical and tobacco history.
Typical examination steps:
- Visual inspection (size, color, borders, location)
- Palpation (soft vs firm, mobile vs fixed)
- Adjacent tissue check (other lesions, white/red patches)
- Lymph node exam (neck swelling, tenderness)
- Medical history (smoking, alcohol, systemic diseases, medications)
Diagnostic tests may include:
- Biopsy (gold standard): remove a small tissue sample under local anesthesia; sent to pathology lab; results in 5 to 7 days; cost NPR 3,000 to 5,000 including lab fee
- Blood tests: CBC, B12, iron, folate for recurrent ulcers
- Viral swab or culture: if infection suspected
If findings suggest systemic disease (immune disorder, Behçet’s disease) or cancer, we refer you to an ENT specialist, oral and maxillofacial surgeon, or oncologist at Tribhuvan University Teaching Hospital, Nepal Mediciti, or Grande International Hospital.
Do not delay investigation out of fear. Most biopsied lesions turn out to be benign (traumatic ulcer, fibroma, hyperplasia), but early cancer detection saves lives. The entire process from first visit to biopsy result takes 7 to 10 days.
Relief, Treatment, and Prevention: A Practical Action Plan
Most uncomplicated ulcers improve with gentle care: avoid spicy/acidic foods, use soothing gels, and consider salt-water rinses while keeping brushing soft and consistent. Dentists may prescribe protective pastes, antiseptic rinses, or anti-inflammatory gels, and they can remove triggers like sharp edges or ill-fitting appliances. If ulcers recur, a prevention plan should include trigger tracking, nutrition checks, and early treatment for cold sore flare-ups.
Safe Home Care and What NOT to Do (Harsh Rinses, Popping Blisters, Wrong Creams, Eye-Touching)
Safe home care speeds healing and prevents complications:
- Saltwater rinse: dissolve 1 teaspoon salt in 1 cup warm water; swish gently for 30 seconds, 3 to 4 times daily (reduces bacteria, soothes pain)
- Avoid irritants: skip spicy, acidic, salty, or rough foods (chips, toast crust) until healed
- Soft diet: dal-bhat with soft vegetables, yogurt, mashed banana, scrambled eggs
- Ice chips: suck on ice to numb pain temporarily
- Over-the-counter gels: benzocaine or lignocaine gel for pain relief (apply with cotton swab, not fingers)
- Maintain hygiene: brush gently with a soft toothbrush; rinse after meals
Critical mistakes to avoid:
- Harsh alcohol mouthwashes: burning sensation without healing benefit; stick to plain saltwater or prescribed antiseptic rinse
- Popping cold sore blisters: increases infection risk, prolongs healing, spreads virus to other areas
- Using steroid cream without diagnosis: worsens viral and fungal infections
- Touching ulcer then rubbing eyes: transfers infection (especially cold sores) to cornea
- Ignoring dental irritants: continuing to wear sharp dentures or braces without adjustment delays healing
Dentist Treatments: Protective Pastes, Antiseptic Rinses, Steroid Gels, Addressing Trauma/Irritants
Professional treatments provide faster relief and address underlying causes:
- Protective pastes (Orabase, Gelclair): coat the ulcer, shield from food/saliva, reduce pain by 50 percent within hours
- Antiseptic rinses (chlorhexidine 0.2 percent): reduce bacterial load, prevent secondary infection, speed healing by 2 to 3 days
- Topical steroid gels (triamcinolone): reduce inflammation in severe canker sores; applied 2 to 3 times daily for 5 to 7 days
- Cautery (silver nitrate): chemical cautery seals nerve endings in painful ulcers, provides instant pain relief (used for major aphthous ulcers)
- Smoothing sharp teeth: remove jagged edges with polishing bur (takes 5 minutes, no anesthesia needed)
- Orthodontic wax: cover braces brackets that rub until adjustment appointment
- Denture relining or adjustment: eliminate pressure points in 1 visit
At BrightSmile Dental Clinic, we also prescribe antiviral medications for cold sores, antifungal treatment for thrush, and perform biopsies when necessary. Treatment costs NPR 1,500 to 3,500 depending on complexity, with follow-up included.
Prevention and “Recurrence Plan”: Trigger Control, Oral Hygiene Tweaks, and a Workup Checklist to Discuss
Prevention strategies cut recurrence by 50 to 70 percent in motivated patients:
Trigger control:
- Switch to SLS-free toothpaste (brands: Sensodyne Pronamel, Himalaya Complete Care)
- Manage stress through adequate sleep, exercise, mindfulness (stress is the top trigger)
- Avoid known food triggers (track with a diary: spicy curries, tomato, citrus, nuts)
- Use lip balm with SPF 30+ to prevent cold sore reactivation from sun exposure
- Stay hydrated (dry mouth worsens ulcers)
Oral hygiene tweaks:
- Brush gently with extra-soft toothbrush (reduces trauma)
- Rinse mouth after eating acidic or spicy foods
- Avoid chewing tobacco, paan, or gutkha (major cancer risk and ulcer trigger)
- Limit alcohol (dries mucosa, increases cancer risk)
Recurrence workup checklist to discuss with your dentist:
- Blood tests: CBC, B12, ferritin, folate, thyroid function
- Dietary review: adequate protein, vegetables, fruits
- Medication review: drugs causing ulcers (NSAIDs, bisphosphonates, chemotherapy)
- Autoimmune screening: if recurrent ulcers plus joint pain, rashes, or eye issues
- Consider suppressive antiviral therapy: if cold sores occur more than 6 times per year
People with frequent mouth ulcers benefit from a personalized prevention plan. We help you identify your specific triggers, correct nutritional gaps, and provide maintenance treatments (monthly antiseptic rinses, quarterly check-ups) to minimize flares.
Mouth ulcers are common but not always simple. Most heal within 2 weeks, but persistence, unusual appearance, or red flag symptoms require professional evaluation. You reduce worry and speed recovery by understanding the difference between canker sores, cold sores, and infections, following safe home care, and seeking timely dental or medical advice when warning signs appear.
At BrightSmile Dental Clinic in Putalisadak, Kathmandu, we provide thorough oral ulcer evaluation, biopsy services, and customized prevention plans. Contact us at +977-9748343015 or brightsmileclinic33@gmail.com to book an examination. Early assessment protects your oral health and gives you peace of mind.
How can I tell if it’s a canker sore or a cold sore?
Canker sores appear inside the mouth and are not contagious. Cold sores appear on or near the lips, often start with tingling, and blister before crusting. If unsure, use location and blistering as key identifiers. Cold sores are viral; canker sores are caused by irritation, stress, or deficiency.
Are canker sores contagious?
Canker sores are not contagious and do not spread through kissing or shared utensils. They result from irritation, stress, or nutritional factors, not infection. Seek evaluation if symptoms worsen, spread, or involve fever or swelling.
Are cold sores always herpes?
Most cold sores are caused by herpes simplex virus type 1 (HSV-1), though HSV-2 can also be responsible. Symptoms often start with tingling, followed by clustered blisters. Cold sores are viral, and antiviral treatment, not antibiotics, can reduce symptom duration.
What does an infected mouth ulcer look like?
An infected mouth ulcer may appear red, swollen, painful, and produce pus or a bad odor. Additional signs include fever, swollen lymph nodes, or gum pain. In some cases, it may be due to a dental abscess. Get evaluated if symptoms worsen.
How long should a mouth ulcer take to heal?
Most canker sores heal in 7–14 days. Cold sores usually resolve in 7–10 days. Any mouth ulcer lasting more than 3 weeks requires evaluation to rule out infection or more serious conditions.
When should I worry that a mouth ulcer could be cancer?
Worry if a mouth ulcer lasts over 3 weeks, bleeds easily, feels firm, or has raised edges. Additional signs include neck lumps, numbness, or trouble swallowing. Persistent or unusual sores should be evaluated promptly.
What home remedies actually help mouth ulcers?
Home remedies for mouth ulcers include salt-water rinses, avoiding spicy foods, and using over-the-counter protective gels. Use a soft brush and avoid alcohol-based mouthwash. These reduce pain and promote healing.
Can toothpaste cause mouth ulcers?
Toothpaste with sodium lauryl sulfate (SLS) can cause or worsen mouth ulcers in sensitive individuals. Switching to SLS-free products often reduces flare-ups. Trauma from brushing can also trigger ulcers.
Why do I keep getting mouth ulcers again and again?
Recurring mouth ulcers often result from stress, irritation, or nutritional deficiencies in iron, B12, or folate. Immune or digestive conditions can also play a role. Track triggers and consult a dentist if ulcers are frequent or severe.
Should I see a dentist or a doctor in Kathmandu for mouth ulcers?
See a dentist first for mouth ulcers, especially if caused by teeth, braces, or gum issues. If symptoms suggest infection, medication reaction, or systemic illness, the dentist may refer to a doctor or specialist. Urgent care is needed for severe symptoms or duration over 3 weeks.