Bleeding gums affect 3 out of 4 adults at some point in their lives, yet most people ignore the warning until the damage becomes irreversible. You might assume the blood on your toothbrush is normal or harmless, but it is almost always your body signaling inflammation or infection in the gum tissue. The good news? Early-stage gum disease is reversible with professional cleaning and improved home care, and even advanced cases can be controlled when diagnosed and treated promptly.
At BrightSmile Dental Clinic in Putalisadak, Kathmandu, we see patients daily who could have avoided bone loss, recession, and tooth mobility if they had acted sooner. This guide explains why gums bleed, how to assess the severity at home, and what treatments actually stop the progression, from simple adjustments you can make today to deep cleaning and surgical intervention when necessary.
Bleeding gums: what it means (and when it’s urgent)

Bleeding gums signal inflammation or infection in the tissue, not a normal response to brushing or flossing. Healthy gums remain firm and pink without bleeding, so any blood appearance indicates your body is reacting to irritants like plaque or tartar buildup. You should seek urgent dental care if you notice pus discharge, sudden swelling, loose teeth, or fever accompanying the bleeding.
Is it normal for gums to bleed when brushing or flossing?
Healthy gums do not bleed under normal brushing or flossing pressure. Blood appears when the gum tissue is inflamed, weakened, or infected. The most common trigger is plaque buildup along the gumline, which irritates the tissue and makes it fragile. You might notice pink-tinged saliva after spitting, streaks of blood on floss, or light red spots on your toothbrush bristles.
Occasional minor bleeding can occur if you floss aggressively after weeks of skipping or if you switch to a harder brush, but the bleeding should disappear within 3 to 5 days as tissue adapts. Bleeding that persists beyond one week, occurs daily, or worsens over time indicates inflammation that will not resolve on its own.
Quick self-check: mild irritation vs possible gum disease
Stand in good light and examine your gums in a mirror. Healthy gums are pale pink, firm to the touch, and hug the teeth tightly without gaps. Warning signs of gum disease include:
- Color change: bright red, dark red, or purplish gums instead of pale pink
- Swelling: puffy tissue that bleeds at the slightest touch
- Texture: shiny, smooth surface instead of the normal stippled “orange peel” look
- Recession: roots becoming visible, teeth looking longer than before
- Bad breath: persistent foul odor even after brushing
Gums that bleed only when you press hard or floss roughly, with no other symptoms, usually indicate mild irritation. Gums that bleed spontaneously, feel tender, or show two or more warning signs above suggest gingivitis or early periodontitis.
When to see a dentist urgently (swelling, pus, loose teeth, fever)
Seek same-day or next-day dental care if you experience:
- Pus discharge: white or yellow fluid oozing from the gumline or between teeth
- Sudden swelling: gum tissue ballooning overnight, especially around one or two teeth
- Loose or shifting teeth: teeth that move when you push with your tongue or feel wobbly when chewing
- Fever or malaise: body temperature above 38°C (100.4°F) combined with gum symptoms
- Severe pain: throbbing or sharp discomfort that disrupts sleep or eating
These symptoms suggest an acute periodontal abscess or advanced infection that can spread to surrounding bone and soft tissue. Delaying treatment increases the risk of tooth loss and systemic complications, particularly if you have diabetes or a weakened immune system. Contact BrightSmile Dental Clinic at +977-9748343015 or message us via WhatsApp for priority scheduling.
Why gums bleed: dental causes vs medical contributors
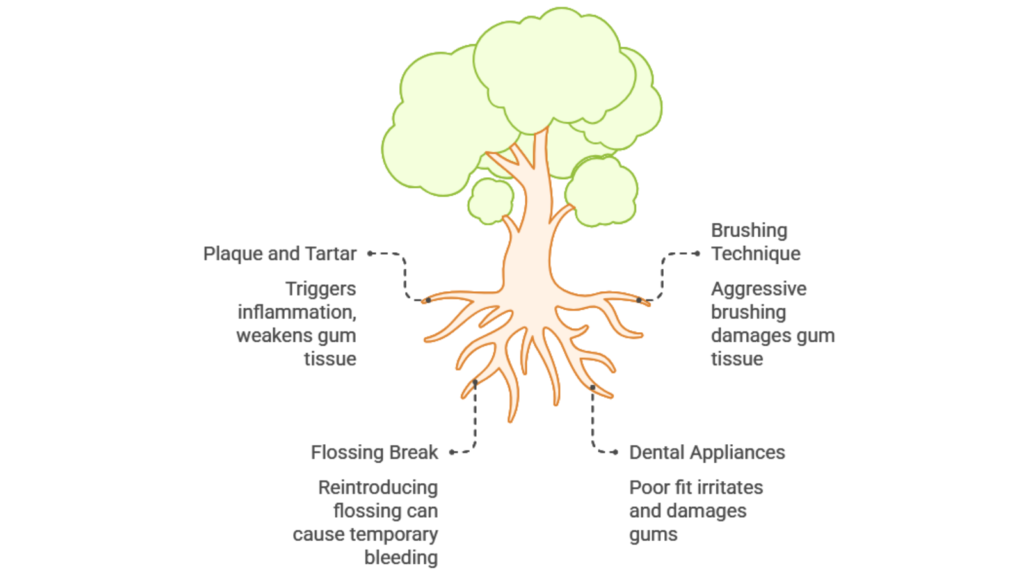
Plaque and tartar buildup along the gumline cause most cases of bleeding gums by triggering inflammation that weakens tissue. Technique errors like brushing too hard, gaps in flossing routines, and poorly fitting dental appliances also contribute to localized bleeding. Medical factors such as pregnancy hormones, uncontrolled diabetes, vitamin deficiencies, and blood-thinning medications can amplify bleeding or slow healing even when oral hygiene improves. The dental causes are:
1. Plaque and tartar buildup (most common cause)
Plaque is a sticky bacterial film that forms on teeth within hours of eating. You naturally produce plaque throughout the day; the bacteria inside it release acids and toxins that irritate gum tissue. Plaque that remains undisturbed for 24 to 72 hours hardens into tartar (calculus), a yellowish or brownish deposit that bonds to enamel and cannot be removed by brushing alone.
Tartar extends below the gumline, creating a rough surface where more bacteria accumulate. The immune system responds by sending white blood cells to the area, causing inflammation, redness, and fragile gum tissue that bleeds easily. This cycle perpetuates itself: tartar holds bacteria in place, bacteria trigger inflammation, and inflamed gums bleed and recede, exposing more root surface for tartar to attach.
Professional scaling removes tartar from above and below the gumline, interrupting this cycle and allowing gums to heal. Most patients notice reduced bleeding within 5 to 7 days after a thorough cleaning.
2. Brushing too hard, wrong technique, or hard bristles
Hard-bristle brushes or aggressive horizontal scrubbing can abrade gum tissue and cause bleeding even in the absence of plaque. The damage appears as gum recession along the outer (cheek-side) surfaces of teeth, especially canines and premolars where people tend to apply extra pressure.
Switch to a soft or extra-soft toothbrush and use gentle circular motions or short vertical strokes. Hold the brush at a 45-degree angle toward the gumline and let the bristle tips do the work; you should feel light pressure, not pain. Bleeding from technique alone typically resolves within 3 to 5 days after correction, but recession caused by years of hard brushing does not grow back without surgical grafting.
3. Flossing after a long break: why bleeding can happen at first
Gums that have not been flossed for weeks or months are often inflamed and edematous (swollen with fluid). The first few flossing sessions can produce noticeable bleeding as the floss disrupts inflamed tissue and dislodges trapped debris. This is a temporary adjustment period, not a reason to stop flossing.
Continue flossing daily with gentle C-shaped motions around each tooth. Bleeding should decrease significantly within 5 to 7 days as inflammation subsides. Bleeding that persists beyond two weeks despite proper flossing indicates tartar buildup below the gumline or early periodontal pockets that require professional cleaning.
4. Braces/retainers/dentures irritation and poor fit
Orthodontic brackets, retainers, and partial dentures create surfaces where plaque accumulates more easily. Metal brackets in particular trap food particles near the gumline, and patients often skip flossing around braces due to difficulty, allowing inflammation to develop.
Dentures that no longer fit properly can rub against gums and cause localized sore spots that bleed. Bone resorption after tooth extraction changes the shape of the jaw ridge over time, loosening dentures that once fit snugly. You will need a reline or replacement every 3 to 5 years on average to maintain proper fit.
Medical contributors: pregnancy hormones, diabetes risk, vitamin deficiency, medication-related bleeding
Pregnancy hormones
Elevated progesterone and estrogen during pregnancy increase blood flow to gums and make tissue more sensitive to plaque. Even small amounts of plaque can trigger exaggerated inflammation, a condition called pregnancy gingivitis, which peaks around the second trimester. Gums become swollen, red, and bleed easily despite good brushing habits.
Pregnancy gingivitis resolves postpartum but requires professional cleanings during pregnancy to prevent progression. Untreated periodontitis in pregnant women has been linked to preterm birth and low birth weight in some studies, though causation is still debated.
Diabetes risk
High blood sugar impairs immune function and slows tissue healing, making gums more vulnerable to infection. People with poorly controlled diabetes (HbA1c above 7%) are 2 to 3 times more likely to develop periodontitis compared to non-diabetics. Conversely, severe gum disease can worsen blood sugar control by increasing systemic inflammation, creating a two-way relationship between diabetes and periodontal health.
Vitamin deficiency
Severe vitamin C deficiency (scurvy) causes gum bleeding, swelling, and tooth loosening, but this is rare in modern diets. Mild vitamin C insufficiency can contribute to delayed healing and fragile gum tissue, particularly in people with restricted diets or malabsorption issues. Vitamin K deficiency affects blood clotting and can cause prolonged bleeding from minor gum trauma.
Medication-related bleeding
Blood thinners (aspirin, warfarin, newer anticoagulants) do not cause gum disease but make existing inflammation bleed more readily. You may notice heavier or longer bleeding after flossing or brushing. Never stop blood thinners without consulting your physician; instead, address the underlying gum inflammation through professional cleaning and improved home care.
Certain medications for high blood pressure (calcium channel blockers like amlodipine) and anti-seizure drugs (phenytoin) cause gingival overgrowth, where gum tissue becomes thick and bulbous, trapping plaque and bleeding easily. Regular dental cleanings and meticulous plaque control are essential for managing this side effect.
Gum disease stages: gingivitis vs periodontitis
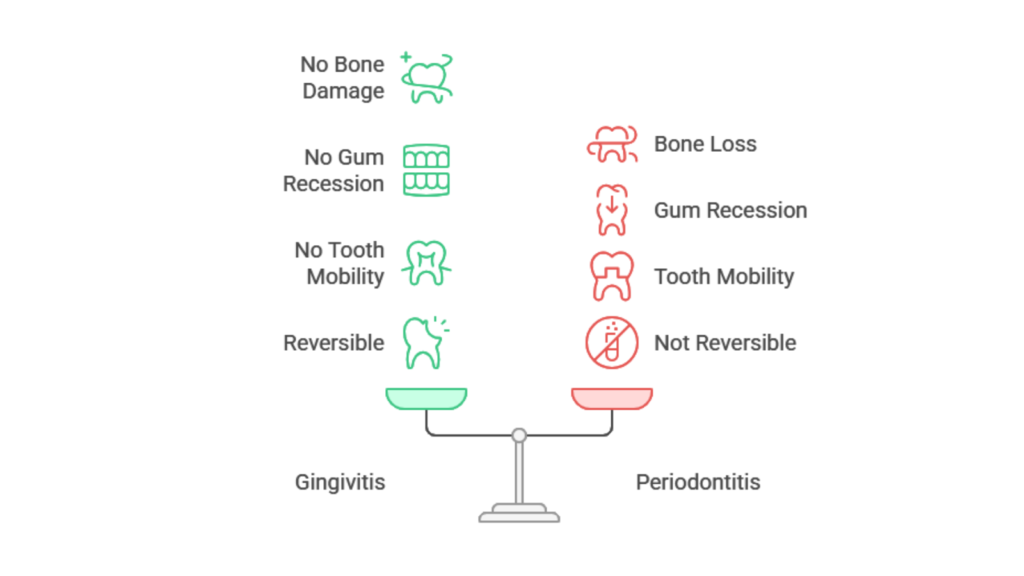
Gingivitis is reversible gum inflammation without bone damage, characterized by redness, swelling, and bleeding that resolve within 1 to 2 weeks after professional cleaning. Periodontitis develops when inflammation destroys the bone and ligament supporting teeth, creating deep pockets, gum recession, and eventual tooth mobility. Ignoring early bleeding allows silent progression from bad breath to bone loss to tooth loss over months or years, making early intervention critical.
Gingivitis: symptoms and why it’s often reversible with early care
Gingivitis is inflammation of the gum tissue without damage to the bone or ligament supporting the teeth. Symptoms include red or swollen gums, bleeding during brushing or flossing, and occasional bad breath. You will not experience pain, tooth mobility, or gum recession in pure gingivitis.
The key feature of gingivitis is reversibility: professional cleaning to remove plaque and tartar, combined with daily brushing and flossing, allows gum tissue to return to a healthy state within 1 to 2 weeks. There is no permanent damage at this stage. Untreated gingivitis, however, can progress to periodontitis in susceptible individuals, particularly smokers, diabetics, and people with genetic predisposition to aggressive gum disease.
Periodontitis: pockets, bone loss, recession, and tooth mobility
Periodontitis occurs when inflammation extends below the gumline and destroys the periodontal ligament and alveolar bone that anchor teeth in the jaw. Dentists measure “pocket depth” with a small probe; healthy gums have pockets of 1 to 3 millimeters, while periodontal pockets of 4 millimeters or deeper indicate bone loss.
As bone recedes, gums follow the bone level downward, exposing root surfaces and creating the appearance of longer teeth. Teeth may become sensitive to cold or touch, and advanced bone loss causes mobility, teeth that shift position or feel loose when chewing. Periodontitis is not reversible in the sense that lost bone does not regenerate on its own, but the disease can be arrested and controlled with deep cleaning, maintenance visits, and surgical intervention when necessary.
What happens if you ignore bleeding gums (bad breath → recession → loose teeth)
Ignoring early bleeding allows gingivitis to progress silently to periodontitis over months or years. The timeline varies: aggressive periodontitis can destroy bone within 12 to 18 months, while chronic periodontitis may take 5 to 10 years to cause significant damage.
The progression typically follows this pattern:
- Bad breath: sulfur-producing bacteria colonize deep pockets, causing persistent foul odor
- Gum recession: bone loss pulls gums downward, exposing sensitive roots
- Tooth sensitivity: exposed roots lack protective enamel and react to hot, cold, and sweet
- Mobility and shifting: teeth move position or tilt as bone support diminishes
- Tooth loss: severely mobile teeth become non-functional and require extraction
Patients often report that they “suddenly” lost a tooth, but the bone loss occurred gradually over years without noticeable symptoms until the final stage. Early intervention stops this cascade before irreversible damage occurs.
Diagnosis at the clinic: how dentists confirm gum disease
Dentists measure pocket depth around each tooth using a periodontal probe, with readings of 4 millimeters or deeper indicating bone loss and active disease. Dental X-rays reveal the height of bone surrounding tooth roots and show destruction patterns that clinical examination alone might miss. Your dentist will also assess risk factors like smoking, diabetes, and family history to tailor treatment and determine appropriate maintenance schedules.
Gum exam and pocket measurements (what the numbers mean)
Dentists use a periodontal probe, a thin metal instrument with millimeter markings, to measure the depth of the gum pocket around each tooth at 6 points (3 on the cheek side, 3 on the tongue or palate side). You will hear the dentist or hygienist call out numbers like “3-2-3” or “5-4-6.”
Here is what the numbers mean:
- 1–3 mm: healthy attachment with no bone loss
- 4–5 mm: early to moderate periodontitis; some bone loss present
- 6 mm or deeper: advanced periodontitis; significant bone destruction
The dentist also checks for bleeding on probing (BOP). Healthy gums do not bleed when gently probed; bleeding indicates active inflammation even if pockets are shallow. A comprehensive periodontal exam records pocket depth, bleeding points, recession, mobility, and furcation involvement (bone loss between roots of multi-rooted teeth).
Dental X-rays for bone level checks
Intraoral X-rays (bitewings and periapicals) show the height of bone surrounding each tooth root. Healthy bone reaches within 1 to 2 millimeters of the cementoenamel junction (the line where the crown meets the root). Periodontitis creates horizontal or vertical bone loss patterns visible as dark areas on X-rays.
X-rays reveal bone loss that clinical probing alone might miss, particularly between teeth or on hidden root surfaces. Dentists compare current X-rays to previous images to assess disease progression and treatment response over time.
Risk factors your dentist will ask about (tobacco, diabetes, past gum issues)
Your dentist will ask about smoking or tobacco use, which is the single strongest modifiable risk factor for periodontitis. Smokers are 3 to 6 times more likely to develop severe gum disease and respond poorly to treatment due to impaired blood flow and immune function in gum tissue.
Other risk factors include:
- Diabetes: especially if HbA1c is above 7%
- Family history: genetic factors influence immune response to bacteria
- Medications: blood thinners, immunosuppressants, medications causing dry mouth
- Stress: chronic stress impairs immune function and healing
- Previous gum disease: recurrence is common without maintenance care
Identifying risk factors helps tailor treatment and follow-up schedules. High-risk patients typically require more frequent cleanings (every 3 months instead of 6).
Treatment options that stop bleeding (step-by-step)

You can reduce mild bleeding immediately by switching to gentle brushing with a soft-bristle brush, flossing daily, and rinsing with warm saline after meals. Professional scaling removes tartar from above and below the gumline for gingivitis and early periodontitis, typically resolving bleeding within one week. Deep cleaning (scaling and root planing) under local anesthesia treats moderate to advanced disease with pocket depths of 5 millimeters or greater, often requiring antibiotics or surgical intervention for cases that fail to heal.
What you can do today: safe steps to reduce bleeding and inflammation
You can begin improving gum health immediately with these evidence-based home measures:
- Brush twice daily with a soft-bristle brush using gentle circular motions along the gumline; avoid hard scrubbing
- Floss once daily with gentle C-shaped motions around each tooth, reaching just below the gumline without forcing
- Rinse with warm saline (1/2 teaspoon salt in 240 ml warm water) after meals to soothe tissue and reduce bacterial load
- Avoid mouthwashes containing alcohol as they dry and irritate inflamed gums; choose alcohol-free antimicrobial rinses if desired
- Stop smoking or chewing tobacco immediately, as continued use prevents healing and accelerates bone loss
Bleeding should decrease within 5 to 7 days if the cause is mild plaque irritation. Bleeding that persists or worsens despite these measures requires professional intervention.
Professional cleaning (scaling): when routine cleaning is enough
Scaling removes plaque and tartar from above and below the gumline using hand instruments or ultrasonic scalers. Routine scaling is sufficient for gingivitis and early periodontitis with pocket depths of 3 to 4 millimeters and minimal bone loss.
The hygienist or dentist cleans each tooth surface, polishes to remove surface stains, and applies fluoride to strengthen enamel. The procedure takes 30 to 60 minutes and causes minimal discomfort in most cases. You may experience slight gum tenderness and sensitivity to cold for 24 to 48 hours afterward.
Expect bleeding to reduce significantly within one week as inflammation subsides. Your dentist will schedule a follow-up exam in 4 to 6 weeks to confirm healing and assess pocket depth reduction.
At BrightSmile Dental Clinic in Putalisadak, routine scaling is priced at NPR 2,000 to 3,000, typically bundled with a full oral examination and polishing. Contact us at +977-9748343015 for transparent pricing and appointment scheduling.
Deep cleaning (scaling & root planing): what to expect and healing timeline
Scaling and root planing (SRP) is a non-surgical deep cleaning procedure for moderate to advanced periodontitis with pocket depths of 5 millimeters or greater. The dentist or periodontist cleans tartar from below the gumline and smooths (planes) root surfaces to remove bacterial toxins and encourage gum reattachment.
SRP is performed under local anesthesia to ensure comfort. At BrightSmile Dental Clinic, we apply topical anesthetic gel before injecting to minimize needle discomfort. The procedure is usually completed in 2 to 4 appointments, treating one or two quadrants (sections) of the mouth per visit.
Healing timeline:
- Days 1–3: mild soreness, gum tenderness, and sensitivity to cold; avoid hard or crunchy foods
- Days 4–7: discomfort subsides; gums may appear pink and less swollen
- Weeks 2–4: pocket depths begin to reduce as gum tissue shrinks and reattaches to clean root surfaces
- Weeks 6–8: follow-up probing to measure pocket reduction; most patients see 1 to 2 millimeter improvements
Deep cleaning pricing in Kathmandu ranges from NPR 8,000 to 15,000 for full-mouth SRP depending on disease severity and number of visits required. BrightSmile Dental Clinic offers bundled SRP with follow-up exams at transparent pricing, contact us for a personalized estimate.
Aftercare guide (48 hours and 2 weeks): saline rinses, sensitivity, food tips, what to avoid
First 48 hours after deep cleaning
- Rinse with warm saline (1/2 teaspoon salt in warm water) 3 to 4 times daily to soothe tissue and reduce bacteria
- Avoid hot foods and drinks as gums may be numb from anesthesia; stick to lukewarm or cold temperatures
- Eat soft foods: yogurt, dal, mashed potatoes, scrambled eggs, smoothies
- Avoid crunchy or hard foods: chips, raw vegetables, tough meat, crusty bread
- Skip alcohol and tobacco entirely during healing to prevent irritation and delayed recovery
- Use a soft toothbrush gently; avoid the treated area for the first day, then resume gentle brushing on day two
Two-week maintenance
- Resume normal brushing and flossing by day 3 to 4, but continue gentle technique
- Expect mild sensitivity: use desensitizing toothpaste (e.g., containing potassium nitrate) if cold air or sweet foods trigger discomfort
- Avoid sticky or hard foods (toffee, nuts) until gums feel firm again
- Continue saline rinses twice daily until bleeding and swelling fully resolve
- Attend follow-up appointment at 4 to 6 weeks so your dentist can measure healing progress
Advanced periodontitis: antibiotics (when appropriate), surgery options, referral to a periodontist
Antibiotics
Systemic antibiotics (e.g., amoxicillin, metronidazole) are sometimes prescribed alongside SRP for aggressive periodontitis or acute infections with pus and swelling. Antibiotics alone do not cure gum disease; they only supplement mechanical cleaning by reducing bacterial load temporarily. Overuse contributes to antibiotic resistance, so dentists reserve antibiotics for specific clinical scenarios.
Topical antibiotics (e.g., doxycycline gel placed in deep pockets) may be used as an adjunct in isolated areas that fail to heal after SRP.
Surgical options
Pockets deeper than 6 millimeters or areas with complex bone loss may require periodontal surgery:
- Flap surgery: gum tissue is lifted to allow direct access to deep tartar and root surfaces; bone is reshaped if necessary, then tissue is sutured back in place
- Bone grafts: synthetic or natural bone material is placed in areas of severe bone loss to encourage regeneration
- Gum grafts: tissue from the palate or a donor source is placed over exposed roots to cover recession and reduce sensitivity
- Guided tissue regeneration: membranes are placed between gum and bone to encourage bone regrowth in specific sites
Referral to a periodontist
Your general dentist may refer you to a periodontist (gum disease specialist) if you have:
- Pockets deeper than 7 millimeters despite SRP
- Rapid bone loss or aggressive disease progression
- Complex anatomical issues (furcation involvement, deep vertical defects)
- Need for surgical regeneration or grafting
Periodontal surgery costs in Kathmandu range from NPR 20,000 to 60,000 per quadrant depending on complexity. BrightSmile Dental Clinic collaborates with experienced periodontists in Kathmandu for referrals when advanced care is needed.
Prevention & long-term maintenance (keep it from coming back)
A consistent daily routine of gentle brushing twice, flossing once, and saline rinsing helps heal inflamed gums and prevent recurrence within 7 to 14 days. Essential tools include a soft toothbrush, interdental brushes for wide spaces, and water flossers to supplement traditional flossing around implants or braces. Periodontal maintenance cleanings every 3 to 4 months are critical for patients with gum disease history, as bacteria recolonize faster in treated areas and standard 6-month intervals prove insufficient to prevent relapse.
A simple 7-day gum recovery routine (beginner-friendly)
This daily routine helps heal inflamed gums and prevent recurrence:
Morning (after breakfast):
- Brush gently for 2 minutes with a soft toothbrush and fluoride toothpaste
- Floss between all teeth using gentle C-shaped motions
- Rinse with warm saline (1/2 teaspoon salt in 240 ml water) for 30 seconds
Afternoon (after lunch, if possible):
- Rinse mouth with plain water or saline to dislodge food particles
Evening (before bed):
- Brush gently for 2 minutes
- Floss all teeth
- Rinse with warm saline for 30 seconds
- Optional: apply desensitizing toothpaste to sensitive areas with a clean finger
Daily habits:
- Drink water throughout the day to wash away food and bacteria
- Avoid sugary snacks between meals
- Stop smoking or tobacco use completely
Most patients notice reduced bleeding within 5 to 7 days. Gums should appear firmer and pinker by day 10 to 14. Bleeding that persists beyond two weeks indicates tartar buildup requiring professional cleaning.
Best daily tools: soft brush, interdental brushes, floss/water flosser
Toothbrush
Choose a soft or extra-soft bristle brush with a small head that fits comfortably in your mouth. Replace the brush every 2 to 3 months or sooner if bristles fray. Electric toothbrushes with pressure sensors help prevent over-brushing but are not essential; manual brushing with proper technique is equally effective.
Floss
Waxed floss glides more easily between tight contacts, while unwaxed floss is thinner and may be preferred for very tight spaces. Floss picks or holders are convenient alternatives if traditional floss is difficult to maneuver. Use 30 to 40 cm of floss per session, winding it around your middle fingers and using a fresh section for each tooth.
Interdental brushes
Small cone-shaped or cylindrical brushes that fit between teeth are ideal for wide spaces, implants, or areas under bridges. They clean effectively where floss cannot reach. Choose a size that fits snugly without forcing; multiple sizes may be needed for different gaps in your mouth.
Water flosser
Water flossers (e.g., Waterpik) use pulsating water to dislodge food and plaque along the gumline and between teeth. They are particularly helpful for people with braces, implants, or difficulty using traditional floss. Water flossers supplement but do not replace manual flossing, as they do not remove adherent plaque as effectively as physical contact.
Periodontal maintenance visits: why follow-ups matter after treatment
Periodontal maintenance cleanings are scheduled every 3 to 4 months for patients with a history of gum disease. Standard 6-month intervals are insufficient for people who have had periodontitis, as bacteria recolonize pockets and tartar reforms more quickly in treated areas.
Maintenance visits include:
- Pocket depth measurements to detect early signs of disease recurrence
- Scaling to remove new tartar buildup before pockets deepen
- Polishing and fluoride application
- Review of home care technique and reinforcement of brushing/flossing habits
Research shows that patients who adhere to 3- to 4-month maintenance schedules maintain stable pocket depths and low bleeding scores long-term, while those who skip appointments or revert to 6-month intervals experience recurrence and progressive bone loss.
BrightSmile Dental Clinic in Putalisadak, Kathmandu, offers periodontal maintenance programs tailored to your risk level and treatment history. Contact us at +977-9748343015 or email brightsmileclinic33@gmail.com to schedule your next cleaning and protect the investment you made in your gum health.
Final Thoughts
Bleeding gums are not a minor inconvenience you should tolerate, they are a direct signal that inflammation or infection is damaging the tissue and bone supporting your teeth. Early action prevents irreversible bone loss, recession, and tooth mobility. Professional cleaning removes the tartar your toothbrush cannot reach, and improved daily habits keep inflammation from returning.
Most cases of gingivitis resolve completely within two weeks of treatment, and even moderate periodontitis can be controlled with deep cleaning and regular maintenance. The key is acting before symptoms progress to advanced stages where surgical intervention becomes necessary.
If you are experiencing bleeding gums, gum swelling, bad breath, or sensitivity, schedule a comprehensive gum exam at BrightSmile Dental Clinic in Putalisadak. We offer transparent pricing, gentle care, and evidence-based treatments that stop disease progression and restore gum health. Call +977-9748343015 or message us on WhatsApp to book your appointment today.
Why do my gums bleed when I brush?
Gums bleed when brushing due to plaque buildup that irritates the gum line and causes inflammation, known as gingivitis. Brushing too hard, using a hard-bristle brush, or starting to floss again can also cause bleeding. If bleeding lasts more than 1–2 weeks, seek a professional dental cleaning and evaluation.
Is bleeding gums always gum disease?
Bleeding gums are most often caused by gum disease, but other causes include aggressive brushing, poor dental appliances, pregnancy, vitamin deficiency, or blood thinners. Persistent symptoms suggest gum disease.
How do I know if it’s gingivitis or periodontitis?
Gingivitis causes puffy, bleeding gums without loose teeth. Periodontitis causes gum recession, deep pockets, pus, and loose teeth. Dentists confirm diagnosis through gum measurements and X-rays.
Can bleeding gums go away on their own?
Bleeding gums can stop with improved brushing and daily plaque removal. If tartar is present, professional cleaning is needed. Skipping flossing worsens inflammation.
What can I do at home to stop bleeding gums safely?
Stop bleeding gums by brushing gently with a soft brush, flossing daily, rinsing with salt water, and avoiding irritants. Seek urgent care if severe symptoms appear.
Do gums bleed after a dental cleaning or deep cleaning?
Gums may bleed lightly after cleaning due to sensitivity. Deep cleaning can cause soreness and mild bleeding, which should improve in days. Contact your dentist if symptoms worsen.
What is scaling and root planing, and when do I need it?
Scaling removes plaque and tartar. Root planing smooths root surfaces to allow gum reattachment. Deep pockets, bleeding, or bone loss indicate the need for treatment.
Can gum disease be cured permanently?
Gingivitis can be cured with cleaning and care. Periodontitis is managed by stopping progression and maintaining oral health. Some damage may be permanent.
Are bleeding gums linked to diabetes or other health issues?
Diabetes, vitamin deficiencies, and blood thinners can increase gum bleeding. Frequent bleeding plus other symptoms should be discussed with both a dentist and doctor.
When should I see a dentist for bleeding gums?
See a dentist if bleeding lasts beyond 1–2 weeks. Seek care sooner if you have swelling, pus, bad breath, or loose teeth. Urgent care is needed for fever or facial swelling.